How — and why — to fit more fiber and fermented food into your meals

UTI in older women: Why postmenopausal women are susceptible to urinary tract infection, and what to do about it

Can a routine vaccine prevent dementia?

Some adults may need a measles booster shot. Who should get one and why?

Less butter, more plant oils, longer life?

Healthier planet, healthier people

Counting steps is good — is combining steps and heart rate better?

Appendix pain: Could it be appendicitis?

Can saw palmetto treat an enlarged prostate?

How does Ozempic work? Understanding GLP-1s for diabetes, weight loss, and beyond
Diseases & Conditions Archive
Articles
Eczema tied to higher bone fracture risk
News briefs
Eczema is a common and chronic inflammatory condition that leaves skin dry and itchy. A large study published in the February 2020 issue of The Journal of Allergy and Clinical Immunology found that people with eczema had an increased bone fracture risk, especially if the eczema was severe. Researchers compared 500,000 adults with eczema to more than 2.5 million people who didn't have eczema. Over a period of five years, people with eczema appeared to have slightly higher rates (7% to 18%) of wrist, hip, pelvis, and spine fractures, compared with people who didn't have eczema. People with severe eczema had much higher rates of hip fractures (50% higher), pelvis fractures (66% higher), and spine fractures (109% higher, or more than double the risk) than people without eczema. The study is observational and doesn't prove that eczema causes bone fractures; it could be that certain medications and lifestyle habits contributed to broken bones in the study. "But based on the findings, people with eczema should be aware their skin condition may increase the risk for osteoporosis and bone fractures, and should talk to their health care provider to decide if preventive measures and screening tests for osteoporosis are warranted. Healthy lifestyle choices, such as getting enough calcium and vitamin D and getting regular aerobic and weight-bearing exercise, are important for everyone and may be particularly important for people with eczema," says Dr. Robert Shmerling, a rheumatologist at Harvard-affiliated Beth Israel Deaconess Medical Center.
Image: © PeopleImages/Getty Images
Should I be concerned about my fainting spell?
Ask the doctors
Q. I had a fainting spell the other day. Should I be concerned? What should I do?
A. Fainting, which your doctor may refer to using the medical term syncope, is not uncommon. Experts say as many as one in three adults experiences at least one fainting spell over time. In most cases, it's not related to a serious medical condition, but if you faint, you should always get an evaluation by a doctor to rule out more serious causes, including heart-related problems.
5 ways to dodge incontinence
Most people take bladder control for granted — until the unintended loss of urine interrupts the ability to carry on an ordinary social and work life.
Often, the causes of incontinence are out of a person's control. For example, in women, incontinence is a common side effect of childbirth. For men, it's often a side effect of treatment for prostate problems.
What you need to know about COVID-19 if you have diabetes
Some data suggest that people with diabetes who get COVID-19 are more likely to have serious complications or to die. If you have diabetes, you need to take steps to reduce your risk of getting sick.
Red, brown, green: Urine colors and what they might mean
Departures from the familiar yellow color of urine are often harmless but should be discussed with a doctor.
Most of the time, urine is a pale-yellow color because it contains urochrome, one of the substances produced when hemoglobin gets broken down. Hemoglobin is the protein in red blood cells that sticks to oxygen so it can be ferried around the body.
Occasionally, though, urine turns a very different color. Men may notice the change as their urine enters the toilet bowl or urinal. Women may be more likely to observe it after wiping. Seeing red or orange instead of the usual yellow can be alarming, especially if there are also symptoms like a burning sensation or pain with urination. The alarm may be justified: an abnormal urine color can be an early sign of a serious medical condition. To be on the safe side, it should be discussed with a doctor or another clinician.
Sarcoidosis
What Is It?
Sarcoidosis is an illness that causes tiny islands of inflammatory cells to form throughout the body. These microscopic groups of cells are called granulomas. They are especially common in the lungs, lymph nodes, skin, eyes and liver. The cause of sarcoidosis is unknown.
Sometimes, these granulomas cause very little damage, so a person with sarcoidosis does not have any symptoms of illness and may not even know they have it. In other cases, however, the granulomas produce large areas of inflammation and scarring that can interfere with an organ's normal functions. Although most people with sarcoidosis eventually recover, a few develop forms of the illness that are long-lasting (chronic) and get worse with time.
Are varicose veins a health risk?
Ask the doctors
Q. I have a lot of varicose veins. Do they present any sort of a health risk?
A. Varicose veins are typically viewed as a mild, non-life-threatening condition that is more of a cosmetic annoyance than a serious health problem. That said, varicose veins can be associated with some health-related issues, such as swelling in the legs, blood clots, or damage to the skin caused by pressure from the veins. They may also make you more prone to skin damage, infections, and ulcers.
Allergic rhinitis: Your nose knows
Allergic rhinitis, commonly called hay fever, can be a minor seasonal nuisance or a troubling year-round problem. Most people can find relief by taking an antihistamine and by avoiding the allergens that trigger the irritation.
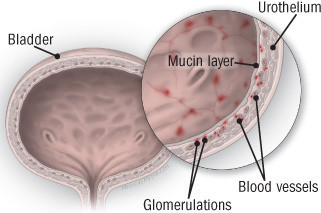
Diagnosing and treating interstitial cystitis
Also called painful bladder syndrome, this frustrating disorder disproportionately affects women.
Interstitial cystitis is a chronic bladder condition that causes recurring bouts of pain and pressure in the bladder and pelvic area, often accompanied by an urgent and frequent need to urinate — sometimes as often as 40, 50, or 60 times a day, around the clock. Discomfort associated with interstitial cystitis can be so excruciating that, according to surveys, only about half of people with the disorder work full-time. Because symptoms are so variable, experts today describe interstitial cystitis as a member of a group of disorders collectively referred to as interstitial cystitis/painful bladder syndrome. (In this article, we'll call it interstitial cystitis, or IC.)
Among the one to two million Americans with IC, women outnumber men by as much as eight to one, and most are diagnosed in their early 40s. Several other disorders are associated with IC, including allergies, migraine, irritable bowel syndrome, fibromyalgia (a condition causing muscle pain), chronic fatigue syndrome, and vulvodynia (pain or burning in the vulvar area that isn't caused by infection or skin disease).

How — and why — to fit more fiber and fermented food into your meals

UTI in older women: Why postmenopausal women are susceptible to urinary tract infection, and what to do about it

Can a routine vaccine prevent dementia?

Some adults may need a measles booster shot. Who should get one and why?

Less butter, more plant oils, longer life?

Healthier planet, healthier people

Counting steps is good — is combining steps and heart rate better?

Appendix pain: Could it be appendicitis?

Can saw palmetto treat an enlarged prostate?

How does Ozempic work? Understanding GLP-1s for diabetes, weight loss, and beyond
Free Healthbeat Signup
Get the latest in health news delivered to your inbox!
Sign Up